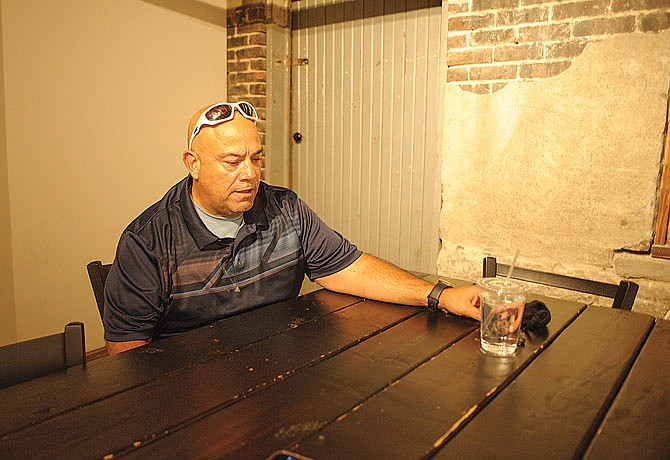
David Rosado didn't know he had a mental illness until he received a diagnosis of schizoaffective disorder about four years ago, when he was in his mid-50s.
What he did know is that when he interacted with public safety officials, those instances were "explosive."
"There'd be no rhyme or reason - really logic," the Cairo, Missouri, man said. "It wasn't hard to find a police officer who was just asking for basic to follow these instructions to be a problem."
Officers couldn't communicate to him what they wanted from him. And, when he was in a crisis, he couldn't communicate with officers.
"When I'm struggling, when I'm having episodes, my ability to communicate - especially in high-amped situations - is impossible," Rosado said. "I had a completely innocent scenario when police made a basic stop - and it could have turned out a whole lot worse than it was. It still resulted in me in the street yelling at police, and there was no reason for it."
It was all because he was not aware of what he was experiencing as it was happening, Rosado said, "and it just snowballed out of control."
Often, the first professional a person sees during a mental health crisis is a law enforcement officer.
The outcome of that encounter may depend on whether the officer has the training to recognize the person may have a mental illness, according to Gena Terlizzi, executive director of the National Alliance on Mental Illness - Missouri.
"Public safety is the first connection to mental health services that people get," she said. "It is hard sometimes to determine if someone is experiencing psychosis or mental illness. (Police officers) are in those situations frequently, and that is challenging for them."
The people undergoing a crisis may not be able to follow basic instructions, she said.
Rosado said he now understands that; and as an "In Our Own Voice" speaker for NAMI Missouri, he shares those experiences with public safety officials undergoing Crisis Intervention Team training.
The NAMI Missouri connection helps officers manage situations they may find themselves in.
The CIT program, developed in Memphis about 30 years ago, is a community partnership of law enforcement, mental health and addiction professionals, hospitals, individuals living with mental illness or addiction disorders, their families, and other community advocates, according to CIT International.
A goal for the Jefferson City Police Department would be to have all 90 sworn officers receive the training, even though the program is voluntary, said Sgt. Joseph Matherne, JCPD's CIT coordinator. The department currently has about 15 officers who have completed the program.
"When somebody goes through a mental health crisis, it's better to get them help than take them to jail," Matherne said. "Jail does not benefit them."
CIT officers learn to identify issues, communicate with the people they come into contact with and connect them with helpful resources, he said.
Keeping in mind "de-escalation" is emphasized during the 40-hour training, the local CIT council follows state guidelines and determines which classes are used, Matherne said. The local council includes law enforcement agencies from Cole, Camden, Laclede, Miller and Osage counties.
"We usually do about eight hours of de-escalation in our training - that deals with how to talk to people," Matherne said. "How to deal with people that are maybe going through a mental health crisis and not triggering things that may make it worse."
The training includes four hours of role play, in which people take officers through scenarios they may face in the field.
Missouri has become a leader in efforts to equip law enforcement agencies to respond to someone undergoing a crisis. In 2013 and 2014, then-Gov. Jay Nixon created a strategic Strengthening Mental Health Initiative to help communities identify and care for Missourians with mental illness. Efforts of the initiative began to connect Community Health Centers with local law enforcement agencies through use of mental health liaisons - mental health professionals who work directly with law enforcement to provide services when needed. The initiative also emphasized the need to provide training so the agencies could create their own regional CIT.
Before Nixon's initiative, local agencies all had different training to deal with people in crisis, according to Perry County Sheriff's Office Detective Jason Klaus, the Missouri CIT coordinator. Scope of training, or whether an agency had training at all, oftentimes depended on what they could afford.
The initiative brought in folks from the Missouri Department of Public Safety to provide on-site technical support and to complete certification paperwork and set aside grant funding to assist with training costs, including supplies.
Public safety organizations are usually the first people to respond when a crisis occurs, Klaus said. Law enforcement should be the first level of response, not the emergency room, he said.
In today's narrative, the last thing people in crisis may want is to call law enforcement, he said.
Police violence against Black people has sparked demonstrations across the nation this year. The recording of the death of George Floyd at the hands of a Minneapolis police officer created outrage, as did the death of Breonna Taylor and the subsequent decision that Louisville officers who killed her would not face charges.
So it's extremely important law enforcement personnel regain community trust and the trust of family members so they may "de-escalate a family's loved-one," Klaus continued.
And, when they know they have a loved one who is going through a crisis, family members are advised to ask for a CIT-trained officer when they call in law enforcement.
Many departments allow their CIT officers to wear a pin identifying them as such, Klaus said. The standardized pin (a blue circle containing the words "Crisis Intervention Team Missouri," with the shape of the state in the center) is intended to be easily seen.
"If an individual is in a crisis and they've had a good response from an officer, they look for that CIT pin," Klaus said. "If you know to look for that pin, you look for it right away."
It takes a long time to build that trust, he said.
Additionally, local councils may customize training sessions to include courses they feel may suit their communities, such as one focused on veterans facing mental health crises.
In those courses, officers may learn what resources are available for veterans. The state council is finalizing the curriculum for a course that would help prevent them from landing in jail.
"We want to get them out of the criminal justice system. They are warehoused in the jail system, not getting appropriate treatment, not getting appropriate medications," Klaus said.
The Council of State Governments released a report in 2018 that points out the resources of government, law enforcement and health care providers combined won't be enough to prevent repeated responses for some individuals.
"Even the most effective law enforcement responses cannot succeed without mental health services that provide immediate crisis stabilization, follow up and longer-term support," the Police-Mental Health Collaborations report says.
Collaborations contain formal commitments between law enforcement, mental health providers and organizations representing people living with mental illness and their families, and can help build on the success of police mental health training, the report says.
The initiative that created mental health councils across the state also set up Community Mental Health Liaisons. The CMHLs are mental health professionals who work out of community health centers. They strengthen the partnerships between community mental health centers, law enforcement and courts to prevent unnecessary jail, prison and hospital stays.
They also free up officers from multiple calls, Sgt. Matherne said.
Among the most important roles of a CIT is to connect a person in crisis with resources. One of those resources is the liaison, he said.
More information about liaisons is available on the Department of Mental Health website at dmh.mo.gov/mental-illness/programs/liaisons.
If a person is in a mental health crisis and dispatchers are aware, dispatchers will contact a CIT, such as Matherne. Matherne calls the local liaison, who may intervene.
"(The liaison) works with that person and says, 'If you have this issue going on, don't call the police, call me.' Now, that person doesn't call (police) at all," Matherne said.
The person calls the liaison. There have been cases when an individual might call the police 10 times a week, who now doesn't call the police, Matherne said.
"That has freed us up to not be tied up on on a mental health crisis," he said.
Laura Heitmann, the liaison with Arthur Center Community Health, in Mexico, said Missouri's resources for responding to mental health crises have come a long way in seven years.
"How do we help folks who show up at hospitals, emergency rooms, mental health centers and police stations? How do we resolve crises with those people so they get the help they need?" she asked.
What has developed, Heitmann said, are community health center staff, people with lived experiences, agencies and others all coming together regularly to discuss how their community is helping people in crisis.
"My sole focus is to work with law enforcement and court systems to insure that people with behavioral health issues are getting directed toward the mental health system and away from the criminal justice system, if possible," she said. "It doesn't mean that people aren't being held accountable for a crime or act."
She might be able to help address the root cause of why someone committed an act. For example, if someone with a substance use problem may have been caught stealing, she tries to get help dealing with the substance use issue.
"They may not always be willing. I've had doors slammed in my face," Heitmann said.
A growing challenge, Terlizzi said, is the number of juveniles who experience mental health crises.
"2020 has been a challenging year. This has been a challenging time for a lot of people," Terlizzi said. "It has impacted youth in ways even a year ago we could not have imagined."
The barrier of social isolation and reduction of resources are concerning. Alongside that, there had been efforts to make behavioral health services available in schools. And schools were closed so services weren't as accessible.
Throwing juveniles into the mix is an added stressed for CIT officers. CIT officers for juveniles must receive an additional 24 hours of training above (and after) they have had the standard CIT training, Matherne said.
Only one officer in the JCPD has had the additional youth training - Matherne.
"There is an emphasis on getting the city training for resource officers," he said. "Every time we try to have a class, of course, something has happened."
The pandemic, for one, has caused cancellations.
And youth undergoing crises are becoming more and more common, he said.
"I'm talking as young as second- or third-graders we're seeing diagnosed with mental health conditions," Matherne said. "It's tough. You're dealing with a little guy who probably doesn't really know what's going on with himself."
He or she may act aggressively in class or the administrative offices. When parents arrive, the activity doesn't stop, Matherne said. It's horrible, when you're talking about an 8- or 10-year-old, he continued.
"The aggression continues," he said. "You've got parents who are at their wits' end. You talk about limited resources for adults. The resources are even less for a child."
Whether adults or juveniles, in the most demanding cases, one option is a 96-hour commitment to a behavioral health center.
St. Mary's Hospital has a behavioral health wing, but it is for adults. When JCPD is forced to commit juveniles, it takes them to the MU Psychiatric Center, a care facility in Columbia.
"You're limited for youth," Matherne said. "There's a little bit of apprehension to place a child in a mental health bed somewhere, and take them away from a parent."
This article was edited at 8:55 a.m. Oct. 15, 2020, to correct the spelling of Laura Heitmann's last name.