CHICAGO - A dying man grabbing a nurse's wrist, asking if God could save him. A patient celebrating a birthday, delighted to find out her nurse also had a birthday that week. A man with his mask on his chin at a Walgreens.
These moments are etched into the memories of two Chicago nurses who treated COVID-19 patients this year. And it has been a year like no other.
Knowing she would want a record of what she experienced, Northwestern Memorial Hospital nurse Blair Bobier, 30, began keeping a journal. Lindsey Gradone, 34, a Northwestern nurse practitioner in the COVID-19 intensive care unit, felt the same and thought of how her family treasures her grandfather's journal chronicling World War II, so she started her own.
In the beginning, the journal entries referenced a "novel coronavirus," and recounted the stockpiling of toilet paper and how an entire floor was secured for virus patients. In March, Gradone wrote, "Within the past few weeks, it's started to spread globally."
The entries continue as the nurses treat a surge in patients, make call after call to frightened family members and hold the hands of the dying.
"It goes beyond writing as a cathartic exercise," Bobier said. "The written product itself is really important to me as a reminder of what I've been through, and a tribute to my patients and their families, and my co-workers."
Before the pandemic, Bobier would write maybe one page in a journal, every now and again. This year, writing became a way to process what she saw. Even as an oncology nurse used to treating patients who might be dealing with unknowns, COVID-19 brought existential challenges, she said.
Similarly, for Gradone, writing became a way to keep memories alive of patients and their families. To remember them as people, even after they died. Family members sent photos of their loved ones that staffers posted on hospital room doors so nurses could see who they were without intubation, without illness. There were photographs of them on cruises, with their grandchildren, in better times.
"You can't forget what this really means, what these numbers really looked like," Gradone said. "What I've written and shared, it's not unique. Ask every person who's working in a COVID unit and they'll have these same stories. And that's what's heartbreaking."
These are some of the details Gradone will remember when the pandemic is over: A tan line from a wedding ring that was removed. The sound of music playing from an iPad a patient's wife loaded with their favorite songs. Holding the hand of a patient whose family missed his death by moments, telling him he was loved.
Both nurses allowed the Chicago Tribune a lens into their journals. They recount fears and bright spots, like the moment Bobier entered a non-COVID-19 patient's room that was filled with balloons and a half-eaten Mariano's cake.
The number of COVID-19 cases in the intensive care unit "has really exploded," Gradone wrote in April. That same day, she wrote, "It's surreal to see so many people on vents."
She mentioned a friend with colleagues in New York being "completely overwhelmed."
The lines at Trader Joe's reminded Gradone of a panic before a hurricane. She wrote that a family member told her not to be afraid, and she added the Bible verse the person recited: "Do not let your hearts be troubled."
Bobier was frustrated to see people in public spaces without masks. She saw firsthand what happened when someone contracted the virus. She wrote about a man with his mask under his chin as he passed by her in a Walgreens.
She commented that his mask was down, hoping he'd recognize it as a mistake. He told her to "grow up." After this incident, she did not approach people publicly. But she never found a way to stanch the rage she still feels when people mock precautions that could keep them from becoming her patient.
In late summer, Gradone took a break from journaling.
"It's been difficult to keep writing," she wrote in October. "I've been burned out and depressed."
She said it was hard to watch patients be so isolated. Difficult to be the person who heard their final fears and pleas. She said she felt guilty when she issued orders for COVID-19 patients that required a staffer to go into their rooms, further exposing colleagues to the virus.
In September, she wrote, the unit had a string of "really sad deaths."
Recently, Bobier arrived at work and took over care for a patient with the virus. He was dying of cancer, and because he also now had COVID-19, he was transferred from hospice at home with family to being alone at the hospital.
Bobier said she writes to remember. But she will never forget his voice.
"Some of them are burned in my memories," she said in an interview. "His voice, the over and over, 'Please save my life,' it will always be in my memory."
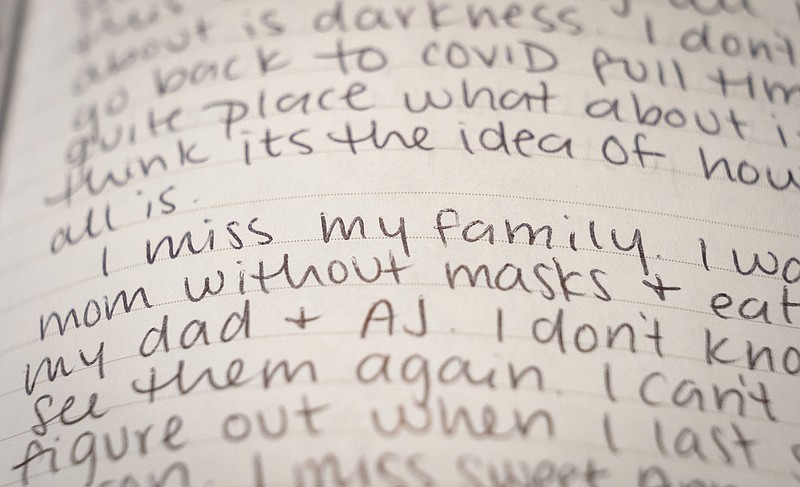
Personally, this time has been difficult for Bobier. She misses her extended family. She said she lost weight because she's not eating at work over her concerns about germs. In October, she wrote about her husband being worried about her.
"He's right," she journaled. "I'm not okay. I'm at a loss for ideas for what will make it better though."
As a new wave of rising cases hit, she wrote, "When I think about this winter coming, all I think about is darkness. I don't want to go back to COVID full time. I can't quite place what about it, but I think it's the idea of how isolating it all is."
"I keep thinking," she wrote, "about the day when I get to go on vacation somewhere with white, white sands and blue, blue water. I'll fall to my knees in the sand and just cry."
When people asked what it was like to work with COVID-19 patients, Gradone was hesitant to share. People seemed interested in the dark details but not much more.
"You don't get to read these stories and go to brunch," she said. "You need to be part of the solution."
Gradone found it increasingly hard to tell family members they couldn't visit patients.
"Last night made me cry," she wrote in a March entry.
She recounted a patient who "looked like a corpse." She discussed end-of-life goals with his son and had to tell him his father could not have visitors. When he was closer to death, the family could say goodbye, but only for a few minutes, and in full protective gear.
She wrote, "We were all tearful in that very quiet, very empty waiting room. I've never gotten so emotional during these conversations."
Just weeks earlier, she'd been at her own grandfather's bedside as he died. She knew, she said, "how important it was to be able to be there, to hold someone's hands."
One of Gradone's patients got COVID-19 from a friend who thought he had allergies. That friend lived, but her patient died.
She wrote, "I got to know him a little bit when he was awake and before he was intubated, but felt like I really found out who he was through talking with his wife."
Another man's kindness was evident from his wife's stories. After he died, the wife called the ICU one more time, even though her husband was no longer there, to hear again he'd had everything possibly done to save him. Gradone could hear vacuuming in the background, as family worked to clean and sell his business.
"They were loved, and even if they didn't do something extraordinary, they shouldn't have died. And it was tragic," Gradone said in the interview. "You just don't want to forget the faces of the people who died from this."
Both nurses spoke to the Tribune on the first day vaccines were rolled out across the U.S. That day, Bobier felt cautiously hopeful, saying it was "surreal."
She said, "I certainly have a lot of hope for it, but we're definitely not out of the woods."
Gradone felt similarly. She knows it will take more than one moment to erase this year.
"It's really emotional," she said. "It's just good to feel some hope that this will end at some point."
Both nurses received a vaccine Dec. 18.