Several nursing homes have pushed back on reports that far fewer than 50 percent of their staff members have received vaccinations against COVID-19.
Some data may have been incorrectly entered into an information system offered by the Centers for Medicare and Medicaid Services (CMS).
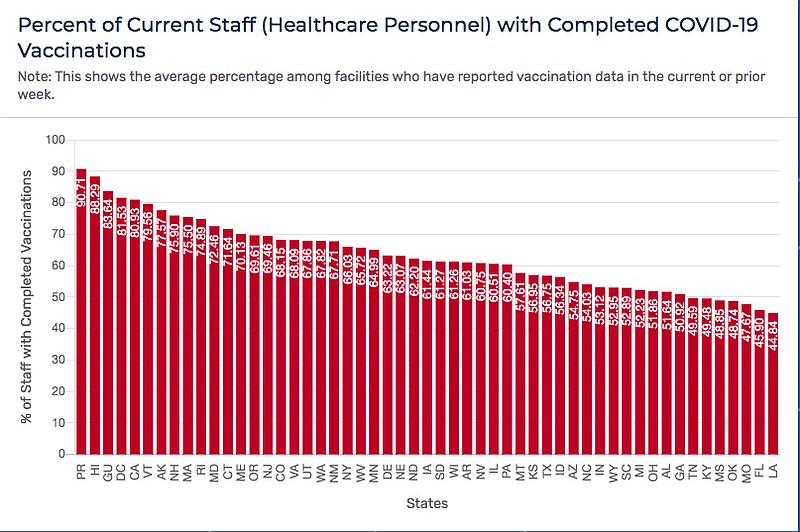
However, CMS remains the best resource to find all this data in one place. And overall, less than 50 percent of staff at Missouri's nursing homes have been vaccinated (47.7 percent), although only 42.8 percent of qualified Missourians have completed vaccinations.
Missouri ranks 48th among states in percentage of nursing home staff members who have completed vaccinations. It is 51st, if the District of Columbia, Puerto Rico and Guam are considered.
So, getting low-paid staff members to accept vaccinations remains a challenge.
Overall, local nursing facilities and the state have done a pretty good job of getting vaccinations for residents. As of Friday, several local nursing facilities, such as River City Living Community, 3038 W. Truman Blvd. (94.6 percent) and StoneBridge Villa Marie, 1030 Edmonds St. (93.8 percent) have maintained vaccination rates higher than 90 percent among residents.
Heisinger Bluffs Lutheran Home, 1002 W. Main St. (85.1 percent); StoneBridge Adams, 1024 Adams St. (89.9); and Oak Tree Villas, A StoneBridge Community, 3108 W. Truman Blvd. (88.5 percent) had maintained rates higher than 90 percent among residents just days before.
However, with turnover of residents, numbers fluctuate daily.
Local nursing facilities' staff members remain above the state average for vaccinations. They also experience fluctuations in completed vaccinations - similar to those that occur in residents, but in smaller increments.
For example, Jefferson City Manor Care Center, 1720 Vieth Drive, showed 51.2 percent of staff were vaccinated early this week. The CMS numbers showed the facility down to 49.4 percent on Friday. StoneBridge Adams, which was at 63.6 percent early this week, climbed to 66 percent Friday.
The current vaccination rate of residents for all StoneBridge facilities Wednesday was 95.2 percent, and 58.6 percent for staff, said Craig Workman, a spokesman for the nursing care provider.
"This compares favorably to the Missouri statewide averages for nursing homes and skilled nursing facilities," Workman said.
The organization does not require vaccinations, but strongly encourages them for residents and staff, he continued. It provides educational materials, posters and promotional videos, and also promotes the Missouri vaccination lottery program.
"We bring our pharmacy's vaccination clinic into each facility every four weeks to promote free onsite vaccinations and answer questions. Despite these efforts, the spread of misinformation on social media and a distrust of government promoting the vaccine are the biggest challenges we see to getting more staff members to accept vaccinations," Workman said.
Facilities report data to the federal government weekly, he said.
While the COVID-19 pandemic may have highlighted staffing issues at nursing facilities, they existed long before the coronavirus took hold, said Steve Bollin, Missouri Department of Health and Senior Services director of licensing and regulation.
Staff at nursing homes are generally a little bit younger than at other health care facilities. They are providing day-to-day care for folks who are otherwise unable to care for themselves or don't have appropriate care at home. And, the pay can be lower than other jobs.
So, turnover can be an issue for nursing facilities.
"There's been a nursing shortage that has been going on for some time," Bollin said. "When COVID-19 hit, staffing was hit by two factors - nurses were attracted to agency staffing, where they were paying higher salaries. And the other was that a lot of staff members who deal with patients were getting sick."
There was already a shortage of patient care assistants (PCA) and Certified Nurse Assistants (CNA), who work directly with patients. By having staff out for extended periods of time by being sick or quarantined, really hit facilities hard.
The financial reimbursement structure is different in long-term care facilities.
"You're providing for basic day-to-day care needs. You're not taking care of an acute illness or an acute injury or something that requires a higher level of care provision or intervention," Bollin said. "It's really more ongoing health maintenance for folks that are unable to care for themselves."
Some are in the facilities for short times. Some for long times. Some for the rest of their lives.
The demands are somewhat less on the nursing staff than would be seen in hospitals.
"It is a hard job. The demands are different," he said.
Across the state, there just aren't enough staff to go around.
Just less than 49 percent of Missouri's nursing home staff members are vaccinated, according to the CMS.
"That is actually consistent with what we have been seeing in general when we have nursing homes or facilities that have outbreaks. We've seen it to be a fairly typical experience that the staffing will be in the 50 percent range," Bollin said, "while residents are in the 90-95 percent range."
His division tracks outbreaks (one case is considered an outbreak) daily, he said. The virulence in nursing facilities has not been as high as it was for the first go-round in COVID-19, he continued.
"Although we're still seeing a pretty significant number. What we're seeing - as the data shows - the greater percentage of it, the last I heard, upwards of 95 percent of the people infected with the delta variant were unvaccinated," Bollin said.
Outbreaks have occurred in residents and staff. A lot of residents have had breakthrough cases. That's not unique to Missouri, he said.
"We have seen that for the residents who have had breakthroughs they tend to have lower acuity of symptoms. They're not as sick," he said. "We're continuing to monitor this very closely. We report this daily as part of our COVID-19 calls. We're keeping a really close eye on how things are happening in nursing homes."
The state monitors nursing facilities by region, he added. However, if there is a significant outbreak at a specific facility, it keeps an eye trained there too. If there is something DHSS can do to help, it will follow up.
Facilities do call DHSS if they need help, he said.
The most common conversation, Bollin said, is about how facilities can find more staff.
Gov. Mike Parson took steps Tuesday to help nursing facilities resolve that issue, when he announced $15 million is to be provided for health care staffing support.
Missouri will commit $15 million to provide health care staffing for all Missouri-licensed or CMS-certified critical access, acute care and long-term care hospitals. Funding will be provided on a firm, fixed staffing rate.
The entire point of the new programs is to make staffing available.
"We have to figure out how this can help long-term care facilities," Bollin said. "They are the next line of care. If (patients) don't need acute care anymore, but they can't go home, they go to a skilled nursing facility, or long-term care facility - the next facility in line until they can go home. If we cannot get folks into there because of staffing issues, that's going to slow down the process. And it clogs things up on the front end - particularly in the emergency department."
DHSS is acutely aware of the challenge.
"It's a whole mix of (conditions), particularly with ICU patients - a lot of them will have been intubated for a couple of days to a week," Bollin said. "Until you find an appropriate place for that person to go to, it causes a logjam and impacts care across the board."