Project managers of the new $2.11 million Fulton State Hospital updated the Missouri Mental Health Commission on Thursday during its regular meeting with details of the new mental health facility. Construction is scheduled to begin in spring 2015, with the hospital to be ready for clients at the end of 2017.
Clients in the maximum-security Biggs Forensic Center will gradually move from Biggs to the new hospital starting in spring 2018.
Bob Reitz, director of psychiatric facilities for Missouri's Division of Behavioral Health, and Drew Henrickson, section leader and senior project manager for the Missouri Office of Administration's Division of Facilities Management, Design and Construction, led the discussion.
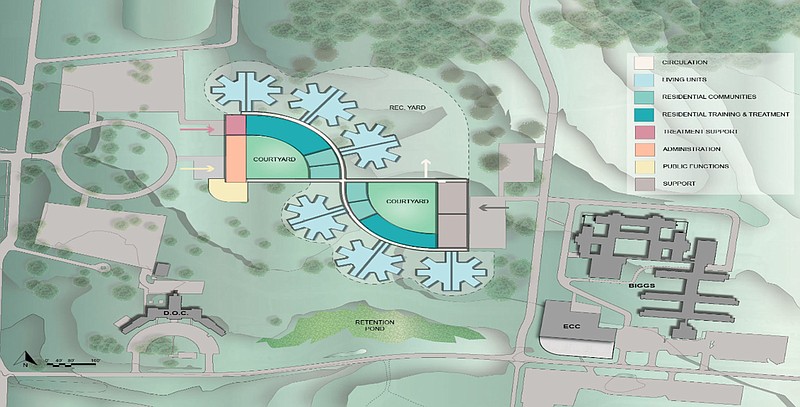
The current concept of a new maximum security building is in the shape of a backward "S" with a hallway cutting through the middle. This will include 300 beds for forensic clients. The current maximum-security facility, Biggs Forensic Center, has 140 beds.
A question was raised if 300 beds is enough, but Rick Gowdy, deputy division director of behavioral health, said the department is "pretty confident" in that number. In 2007, 500 beds were suggested for the new facility.
Keith Schafer, director of the Department of Mental Health, said 500 beds "could not be financially supported," and if there is ever a need for new beds, another new complex may need to be built in the future.
"Hopefully, we won't have to do that," Schafer said.
The concept allows clients in recovery to transition from high security to lower security in the same building. Demolishing the Biggs Forensic Center will be the final phase of the project and is slotted for spring 2018.
Based on the current concept, clients will be housed in 12 living units with 25 beds each, making for a total 300 beds. Living units are connected to residential community spaces and residential training and treatment. Reitz said this will improve safety and maximize the use of staffing.
Whether or not the concept presented results as the final plan, Reitz said it must be flexible for the environment in order to foster future therapeutic practices.
A major addition for the new Fulton State Hospital is a treatment mall.
Treatment malls have become a national standard of practice in mental health facilities, said Dr. Joel Dvoskin, a forensic and clinical psychologist and consultant for mental health institutions across the country. He's been working with Fulton State Hospital administration and project managers on the design team.
A treatment mall, Dvoskin said, gives clients a sense of purpose because they travel from their living unit to another area for various types of treatment - occupational, vocational, etc. The act of going from one place to another also establishes normalcy, Dvoskin said.
"When people wake up in the morning, it's normalizing to get up and go to work or go to school," Dvoskin said.
He said chapels and spaces for exercise are also commonly found in treatment malls.
In the state hospital concept, the treatment mall could have space for services such as haircuts, a convenience-type store for purchasing soft drinks and a recreation center. There may also be a clinic for health care services adjacent to the treatment mall.
Dvoskin advised in the planning of St. Elizabeth's Hospital in Washington, D.C., which was completed in 2010. The work done at St. Elizabeth's was a point of discussion during the meeting, and Reitz referred to St. Elizabeth's as "state of the art."
When administrators were developing a FSH master plan in 2007-08, Reitz and Hendrickson traveled to St. Elizabeth's to see what could be mimicked or improved upon at Fulton.
FSH administrators have echoed the desire for shorter, wider hallways, high ceilings, increased natural light, clear lines of sight and sound reduction (which will be accomplished with construction materials appropriate to a psychiatric facility, according to Mark Stringer, director of the Division of Behavioral Health).
Biggs' current hallways allow for many blind spots, and the ceiling is so low that someone of average height can touch it. Clients have ripped parts of ceiling tiles, exposing piping. The new hospital will be on one level, eliminating stairs, which have been a source for injuries. Dietary services will be included.
One-third of hospital employees file worker's compensation claims, costing $4 million in taxpayer dollars, according to the Department of Mental Health.
"That is an incredibly dangerous situation for our employees," Stringer said.
In his observations of FSH, Dvoskin said it is a "national leader" in its treatment programming, especially with its forensic clients.
"(A new FSH) makes sure that our environment matches our programming," Reitz said.
The architectural design group, Parsons Brinkerhoff, will meet with FSH employees Wednesday through Friday to see what they would like in a new facility.
Mental Health commissioner Steve Roling said the say of employees is vital to the project.
"They're the ones who every day have to deal with this," he said.
Including employees - and clients - in the planning process was a successful component for St. Elizabeth's, Dvoskin said. Their feedback resulted in adjacencies within a building, creating a more convenient flow when moving clients from one space to another.
The closer proximity gave clients increased hours in treatment time, Dvoskin said.
Many suggestions at St. Elizabeth's were in relation to safety, he added, such as eliminating blind spots. There, Dvoskin said the design team was able to balance privacy and dignity with safety and observation.
"If one person can see everyone on the living stations, it allows other people to interact and have treatment," Dvoskin said. "Everybody does better when they feel safe."